You are about to leave a GSK website
You are about to leave a GSK website. By clicking this link, you will be taken to a website that is independent from GSK. The site you are linking to is not controlled or endorsed by GSK and GSK is not responsible for its content.
Whitney’s work. UNRAVELED BY SHINGLES.
The pain during a shingles episode can interfere with a person’s ability to perform daily activities.1
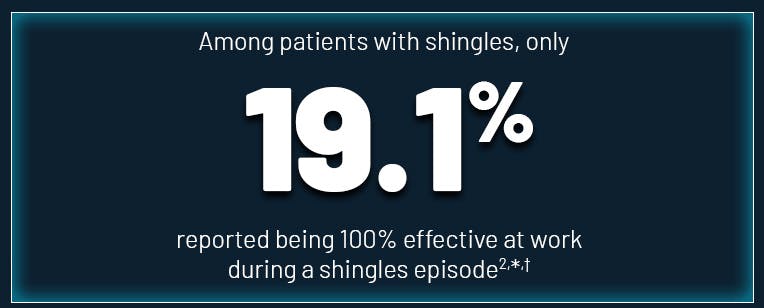
A person's effectiveness at work could be impacted by shingles2
In a cross-sectional survey:
Shingles can result in missed workdays 2
Overall, 43% (334/772) of patients reported missing at least one full day of work (mean = 9 full days) and 29% (227/772) reported missing at least one partial day (mean = 6 partial days) during the shingles episode.2,†
- *
Survey sample size: 695 patients reported effectiveness at work.2
- †
Data from a cross-sectional survey that was administered to 2000 US adult commercial health plan enrollees aged 50 to 64 years with ≥1 HZ medical claim during 2014. Among the 2000 patients, 1018 patients were classified as having severe HZ and 982 as less severe. The survey collected information related to health status (EQ-5D), work productivity, and HZ severity and clinical features. Data regarding absenteeism and presenteeism, was obtained from 772 and 695 individuals, respectively, who completed the survey.2
The pain during a shingles episode could sideline patients from enjoying or fulfilling daily activities1
The pain associated with a shingles episode has been shown to interfere with patients’ ability to perform activities of daily living such as sleeping, walking, and working. Other impacts include relations with others, mood, general activities, and enjoyment of life.1
Shingles and PHN can have a negative impact on a patient’s quality of life affecting physical (eg, chronic fatigue), psychological (eg, anxiety, depression), social (eg, fewer social gatherings), and functional (eg, dressing, bathing) aspects.3
Patients who get shingles could have more frequent doctor and pharmacy visits, which can lead to increased medical costs4
In a real-world healthcare utilization study in adults 50 years and older, during a 1-year follow-up period, patients with shingles had an average:4,‡:

Shingles and shingles-related complications have been associated with increased healthcare costs.
Adjusted annual incremental total all-cause healthcare costs‡ (shingles cohort vs matched non-shingles controls)
- The additional cost for patients with shingles was +$1425 (95% CI: $1397 to $1453)4
- The additional cost for patients with shingles who developed PHN was +$7291 (95% CI: $7125 to $7457)4
- ‡
Data from a retrospective analysis of commercial claims for 142,519 patients ≥ 50 years of age with herpes zoster (HZ) and 357,907 matched controls without HZ assessing incremental all-cause healthcare resource utilization and cost for patients with HZ vs matched controls during the 1-year follow-up period. Controls were matched based on age, sex, and health plan enrollment. Costs were calculated after adjusting for demographic and clinical characteristics. All cost data were adjusted to 2013 US dollars using the medical care components of the US Consumer Price Index.4
“It’s amazing how it affects everything in your life.”
-Sherri, age 55
Real person who had shingles. Other people’s experiences may be different.

Sherri, age 55
“I can’t even describe it. It was, it was absolutely the worst pain I’d ever had.”
-DeAnn, age 55
Real person who had shingles. Other people’s experiences may be different.

DeAnn, age 55
Shingles can lead to potential complications, including PHN3
Share the potential impact of shingles with your patients—see how you and your staff can get the conversation started
References
Curran D, Matthews S, Boutry C, Lecrenier N, Cunningham AL, Schmader K. Natural history of herpes zoster in the placebo groups of three randomized phase III clinical trials. Infect Dis Ther. 2022;11(6):2265-2277.
Johnson KD, Brenneman SK, Newransky C, et al. A cross-sectional survey of work and income loss consideration among patients with herpes zoster when completing a quality of life questionnaire. BMC Health Serv Res. 2018;18(1):662.
Harpaz R, Ortega-Sanchez IR, Seward JF; Advisory Committee on Immunization Practices (ACIP) Centers for Disease Control and Prevention (CDC). Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2008;57(RR-5):1-30.
Meyers J, Madhwani S, Rausch D. Analysis of real-world health care costs among immunocompetent patients aged 50 years or older with herpes zoster in the United States. Human Vaccines and Immunotherapeutics. 2017; 13(8) 1861-1872
